Operative Hysteroscopy: Revolutionizing Women’s Gynecological Care for Better Reproductive Outcomes

In the realm of modern gynecology, technology and expertise converge to offer women less invasive, more precise, and highly effective treatments for various uterine conditions. Among these advancements, operative hysteroscopy stands out as a groundbreaking surgical technique that has transformed the landscape of women’s reproductive health. This detailed guide aims to demystify the procedure, highlight its benefits, and underscore its significance within comprehensive women’s healthcare offered by leading obstetricians and gynecologists.
Understanding Operative Hysteroscopy: What It Is and How It Works
Operative hysteroscopy is a minimally invasive surgical procedure that allows gynecologists to diagnose and treat intrauterine pathologies directly through the cervix, without the need for abdominal incisions. This technique utilizes a slender, high-definition hysteroscope—an optically equipped instrument—that is inserted into the uterine cavity under local or general anesthesia.
The primary goal is to visualize, diagnose, and effectively manage various uterine conditions such as polyps, fibroids, septa, adhesions, and abnormal bleeding sources, thereby improving women’s reproductive potential and overall uterine health. The procedure's remarkable precision minimizes trauma and accelerates recovery, making it a preferred choice for many women and healthcare providers worldwide.
Key Indications for Operative Hysteroscopy
- Uterine Polyps: Small to large growths on the uterine lining that can cause abnormal bleeding and fertility issues.
- Submucosal Fibroids: Benign tumors pressing into the uterine cavity, affecting conception and pregnancy outcomes.
- Intrauterine Septa and Congenital Malformations: Structural anomalies that can interfere with embryo implantation and pregnancy.
- Asherman’s Syndrome: Formation of intrauterine adhesions typically following uterine surgeries or infections, causing infertility or recurrent miscarriage.
- Chronic Abnormal Uterine Bleeding: To identify and remove pathological lesions responsible for persistent bleeding.
- Reproductive Planning and Fertility Enhancement: To prepare the uterine environment for conception by removing obstructive lesions or scar tissue.
The Procedure: Step-by-Step Overview of Operative Hysteroscopy
Preparation and Evaluation
Prior to the procedure, comprehensive preoperative assessments include ultrasound imaging, hysterosonography (Saline Infusion Sonohysterography), and possibly hysterosalpingography to delineate uterine anatomy and pathologies. Blood work and a review of medical history ensure safety and appropriateness for surgery.
Performing the Hysteroscopy
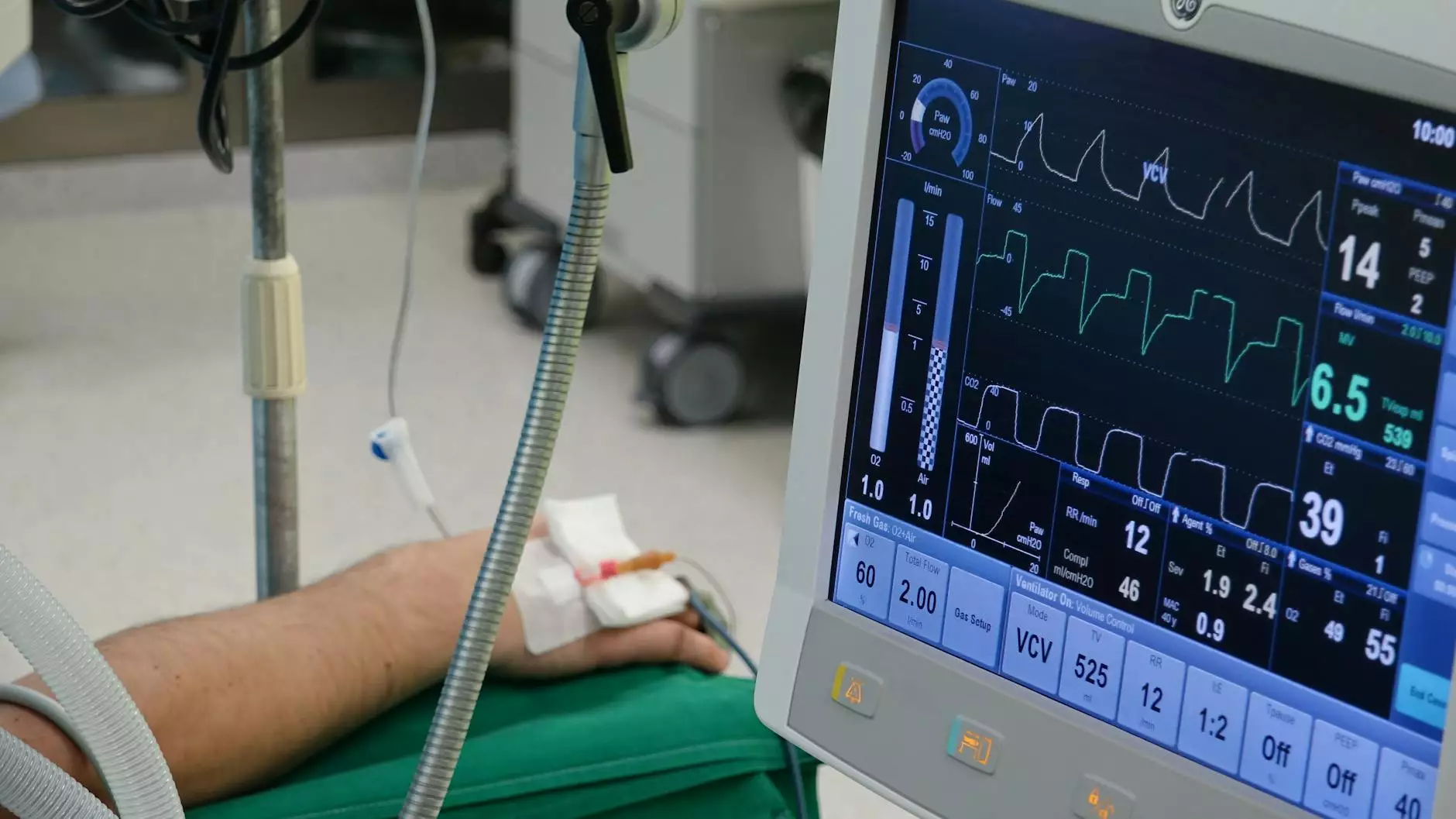
- Anesthesia: The procedure can be performed under local anesthesia with sedation or general anesthesia, based on the complexity and patient preference.
- Insertion of Hysteroscope: The doctor gently widens the cervical canal using dilators if necessary and introduces the hysteroscope coated with sterile saline or CO₂ gas for distention.
- Visualization and Diagnosis: High-definition cameras transmit real-time images to monitors, allowing precise identification of lesions or abnormalities.
- Treatment Approaches: Depending on the pathology, the doctor may introduce miniaturized surgical instruments—such as scissors, laser fibers, or electrosurgical devices—to remove or coagulate lesions.
- Completion and Recovery: Once the targeted pathology is addressed, the hysteroscope is carefully withdrawn. The entire process typically lasts 15-60 minutes, depending on complexity.
Advantages of Operative Hysteroscopy over Traditional Surgical Methods
- Minimally Invasive: No abdominal incisions, reducing trauma, pain, and scarring.
- Enhanced Precision: Direct visualization allows targeted treatment, minimizing damage to surrounding tissues.
- Shorter Recovery Time: Patients often return to normal activities within a day or two.
- Outpatient Procedure: Most operative hysteroscopies are performed on an outpatient basis, avoiding hospital stays.
- Reduced Risk of Infection and Complications: The use of sterile techniques and minimally invasive nature diminish risks associated with open surgeries.
- Fertility Preservation: Removing intrauterine abnormalities can dramatically improve chances of natural conception and successful pregnancy.
Postoperative Care and Follow-Up
After an operative hysteroscopy, patients are advised to rest and may experience mild cramping or spotting for a few days. Pain management with NSAIDs and avoiding strenuous activities during recovery are standard recommendations.
Follow-up visits typically involve ultrasound assessments to confirm the success of the intervention and to monitor healing. In cases of fertility treatments, additional tests or procedures may be scheduled to optimize reproductive outcomes.
Potential Risks and Complications
While operative hysteroscopy is generally safe, awareness of possible risks ensures informed decision-making:
- Perforation of the Uterine Wall: Rare but can occur during instrument insertion or tissue removal.
- Infection: Proper sterile technique minimizes this risk.
- Uterine Adhesions or Asherman’s Syndrome: Postoperative scarring, though less common than with open surgery.
- Fluid Overload or Electrolyte Imbalance: Monitored carefully during the procedure, especially in prolonged surgeries.
Operative Hysteroscopy and Women’s Reproductive Health at DrSeckin.com
At drseckin.com, a dedicated team of top-rated obstetricians and gynecologists specializes in minimally invasive gynecological surgeries, including operative hysteroscopy. Their expertise, cutting-edge technology, and compassionate care ensure that each woman receives personalized treatment tailored to her unique reproductive health needs.
The clinic emphasizes a comprehensive approach—combining accurate diagnosis, state-of-the-art surgical techniques, and continuous follow-up—to optimize fertility outcomes and overall uterine well-being.
Why Choose Expert Care for Your Gynecological Surgery?
- Accurate Diagnosis: Experienced specialists utilize advanced imaging and assessment methods for precise diagnosis.
- Minimally Invasive Expertise: Skilled hands reduce complication risks and promote quick recovery.
- Holistic Reproductive Support: Beyond surgery, they provide counseling, fertility planning, and supportive care.
- Patient-Centered Approach: Respectful communication and tailored treatment plans foster trust and comfort.
- Continuous Innovation: Adoption of the latest techniques ensures state-of-the-art care.
Empowering Women Through Advanced Gynecological Care
Choosing operative hysteroscopy at a reputable center like DrSeckin.com means embracing a future where women regain confidence in their reproductive health, experience fewer complications, and enjoy higher success rates with fertility treatments. This procedure exemplifies how technological innovations, when combined with expert surgical skills, can transform lives, enabling women to achieve pregnancy and improve their overall gynecological health.
The Future of Women’s Gynecology: Continued Innovation and Commitment
The field of gynecology continually evolves with innovations like 3D imaging, robotic assistance, and enhanced hysteroscopic instruments. These developments further improve the safety, efficacy, and patient experience of minimally invasive surgeries such as operative hysteroscopy. Leading clinics, including DrSeckin.com, remain committed to integrating these breakthroughs, providing women with the best possible care for optimal health and reproductive success.
Conclusion: Your Path to Better Reproductive Health Starts Here
In summary, operative hysteroscopy represents a revolution in the management of intrauterine conditions, offering women a safe, effective, and minimally invasive option to address reproductive challenges. Whether you are dealing with abnormal bleeding, infertility-related issues, or congenital abnormalities, consulting a skilled obstetrician and gynecologist who specializes in this advanced technique is essential.
Trust the experts at DrSeckin.com, where cutting-edge technology meets compassionate care, to guide you through your journey toward improved gynecological health and fulfilling your reproductive goals.